Celebrating Universal Health Coverage In Nigeria
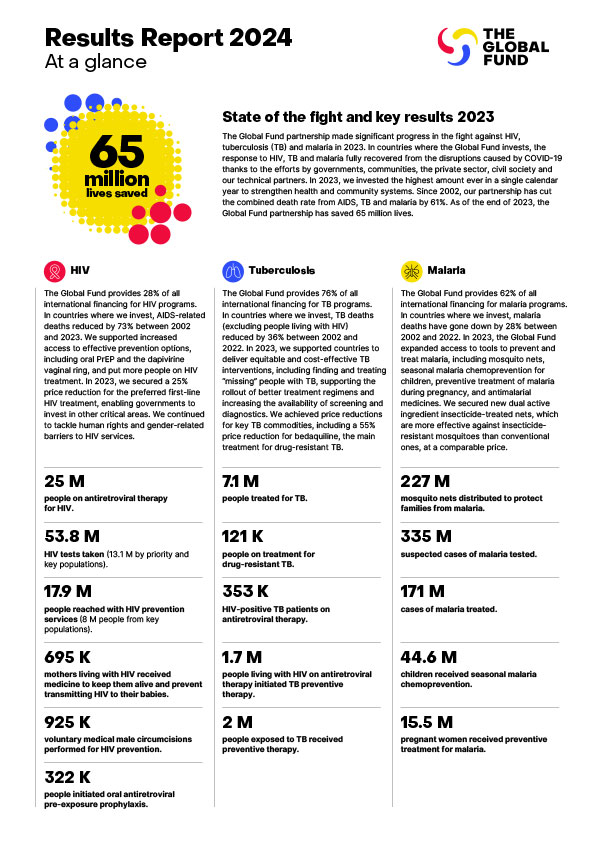
Nigeria is Africa’s most populous nation, with over 200 million people. It’s a vibrant country full of entrepreneurial energy and talent, but it’s also a country affected by poverty and disease. Almost 90 million Nigerians live in extreme poverty. Some 4,000 Nigerians die from malaria every week, mainly small children and pregnant women, 31% of the worldwide total. With close to 2 million people living with HIV, Nigeria has the third highest number of HIV-positive people in the world (after South Africa and India), and the country also has the highest number of people with tuberculosis (TB) in Africa.
That’s why, on Universal Health Coverage Day, I am in Abuja alongside Nigeria’s Coordinating Minister of Health and Social Welfare, Dr. Muhammad Ali Pate, as President Bola Ahmed Tinubu launches Nigeria’s Health Sector Renewal Investment Initiative. This is a bold plan to accelerate Nigeria’s journey towards universal health coverage (UHC), bringing better health and care to every Nigerian. Successful implementation of this plan will require unprecedented collaboration – between Federal and State governments and between the government and development partners, including the Global Fund – plus an unrelenting focus on superb execution and on delivering outcomes. The prize is huge. Given the scale of Nigeria’s population, and the weight of the disease burdens, achieving significant progress here could save millions of lives and shift the global trajectory of the fight against the deadliest diseases, particularly malaria.
The Global Fund will invest over US$1 billion in Nigeria over the next three years (out of some US$15 billion in total), more than in any other country, supporting programs to fight HIV, TB and malaria, and build stronger health systems, all aligned with Nigeria’s overall blueprint for delivering UHC.
Countries Must Invest in Their Own Health Systems to Deliver UHC
Yet in Nigeria, as elsewhere, the key to delivering and sustaining UHC is not external funding, but the commitment of domestic financial resources. No country has achieved UHC without substantial mobilization of domestic resources through taxation or various forms of compulsory health insurance. Nigeria is stepping up its budget commitments towards health and will need to do even more. This is why Nigeria’s reform of the Basic Health Care Provision Fund is a crucial element of the plan.
In many low- and middle-income countries across Africa and elsewhere, there remains a disconnect between the ambition of delivering UHC and the political willingness to mobilize and allocate sufficient public funding to make it happen. In 2001, African Union countries set a target of allocating at least 15% of their budget each year to the health sector – but at no point since then have more than 4 countries ever met it. As recently as February 2023, African leaders recommitted to implementing this Abuja Declaration target. Whether funded through general taxation or compulsory health insurance, UHC entails a more redistributive financial underpinning than many political leaders are prepared to contemplate. It also requires robust and effective systems for resource allocation, financial control and accountability.
Gender and Human Rights Barriers Stand in the Way of UHC
In a worrying number of countries, both rich and poor, there’s also a disconnect around the “U” of UHC, the commitment to universality. It’s impossible for a government to deliver UHC while simultaneously criminalizing or otherwise discriminating against some of the communities most at risk. Policies that reinforce gender inequalities and undermine women’s rights, erode the rights of LGBTQI+ communities, discriminate against refugees and other displaced persons, or deepen inequities in access to health services, are simply incompatible with the notion of UHC.
Reversing the Shortage of Health Workers to Make UHC a Reality
In most countries in Africa, tackling the acute shortage of trained health workers is key to making UHC a reality. Whether it’s community health workers, nurses, doctors, laboratory technicians or other specialists, most African countries face massive gaps. Rich countries aggravate the problem by recruiting tens of thousands of Africa’s most highly skilled health workers to support their own health systems. This means African ministries of health have to be even bolder. For example, Rwanda recently launched an extraordinarily ambitious “4X4” strategy, aiming to quadruple the number of health workers the country trains every year in just four years.
The Global Fund is supporting countries like Nigeria and Rwanda on their journeys towards UHC in multiple ways. Reducing the burden of HIV, TB and malaria saves lives and frees up health system capacity. As the world’s largest multilateral provider of grants for health systems, investing almost US$2 billion per year, we help countries strengthen critical health system components that deliver benefits way beyond infectious diseases. For example, in Nigeria, we are investing in the installation of over 60 oxygen plants at health facilities across the country, saving the lives of mothers and newborns, acute trauma victims, and those needing anaesthetics for surgery. In Rwanda, we’re investing in digital tools for community health workers that will enable them to diagnose, treat and monitor a range of conditions, including non-communicable diseases. We’re also supporting the establishment of new training hospitals to enable the scale-up of health worker training.
While UHC is often described as the objective, arguably it’s more a means than an end, since UHC is how we achieve the ultimate SDG 3 goal of health and well-being for all. So to monitor their progress towards UHC, countries must focus on measurable and human-related outcomes, including disease-specific metrics like reductions in deaths and infections, and overall metrics like life-expectancy and infant, maternal and adult mortality. Moreover, since tackling health inequities is key to delivering the “U” of UHC, it’s imperative to go beyond the averages, to examine and highlight the metrics of the most disadvantaged communities.
Nigeria’s bold plan for UHC – if well executed and sustained – promises to save millions of lives and transform the health of the nation. Consistent with our strategy, the Global Fund is committed to working in close partnership with countries like Nigeria to support the realization of such plans, defeating HIV, TB and malaria, building stronger systems for health, and accelerating the path toward UHC.
This op-ed was first published in Forbes.